
News and Announcements from the CDB
Organ transplantation is an approach considered by medical specialists to replace an organ that can no longer carry out essential physiological functions. Despite many advancements in transplantation research, there are still several hurdles that need to be overcome to improve success rates and access to organ transplantation. Static cold preservation systems are currently used to preserve donor organs prior to transplantation, but they can only maintain the organs in healthy states for a relatively short period—from a few hours to less than a day depending on the organ. Thus, new methods to store organs in healthy conditions for longer periods are needed, as this will improve transplant success rates. There is also a worldwide shortage of organs available for transplantation, as the number of patients waitlisted for organ transplants continues to grow with no corresponding rise in the number of suitable donors or donor organs, necessitating the development of methods to expanding the use of organs from marginal donors, whose organ health may not be considered ideal for transplantation, to increase the donor organ pools.
Now, research associate Jun Ishikawa of the Laboratory for Organ Regeneration (Takashi Tsuji, Team Leader) together with researchers at the Tokyo University of Science, Keio University, and Organ Technologies Inc. have developed a new technique that can preserve donor organs for longer periods and can also resuscitate organs retrieved from donors after cardiac arrest. Using the rat liver as a model organ for transplantation, they reveal a set of culturing conditions that can preserve donor livers for up to two days while ensuring that liver physiological functions are recovered after transplantation. Their findings, published in Scientific Reports, imparts important insights toward establishing an efficient perfusion culture system to extend the storage period of donor organs, as well as to increase the donor organ pool by resuscitating organs donated from marginal donors, such as those who died from cardiac arrest.
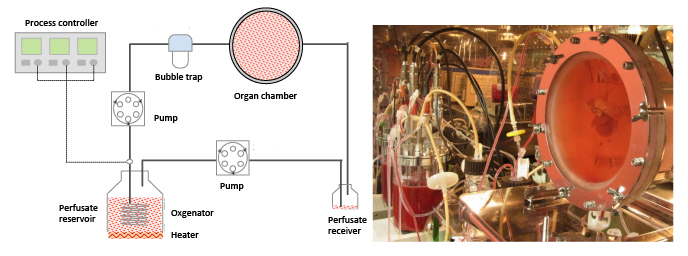
Setup of perfusion culture system. Image on right shows rat liver placed in organ culturing chamber.
Ishikawa and his colleagues first designed a perfusion culture system, which simulates the circulatory system of the body, and placed a liver extracted from a rat into the system’s organ chamber filled with culture medium, ensuring that the entire tissue was sufficiently perfused with medium. The liver was then connected via its portal vein (transports nutrient-rich blood from the gastrointestinal tract) and inferior vena cava (carries de-oxygenated blood to heart) to their perfusion culture system. They tested a range of experimental conditions and found that a combination of cooling the culture to 22°C and adding red blood cells (RBCs), which serves as oxygen transporters, to the culture media maintained liver functions for up to two days as confirmed by measuring concentrations of byproducts of physiological liver functions, such as albumin synthesis, urea, and bile. Under this condition, the levels of alanine aminotransferase, a protein marker indicative of hepatic disorders when high, was low, and tissue structures also remained intact, indicating that liver damage was suppressed. The team also determined that liver cells could survive and recover proliferative abilities after being cooled down to 22°C and then warmed back to body-temperature (37°C) conditions, whereas under other colder temperatures, the cells did not recover proliferative activities or died when returned to 37°C conditions.
Next the group examined whether transplanting a liver cultured in their 22°C perfusion system for 24 hours could replace the function of the recipient’s natural liver. They carried out an auxiliary liver transplantation, and compared effectiveness of using their system with or without addition of RBCs and of using conventional cold storage at 4°C on liver preservation period. Survival rates of rats transplanted with livers stored at 4°C or cultured in perfusion system without RBCs dropped dramatically after transplantation, whereas recipients of livers cultured in perfusion system with RBCs all survived. Seven days after the transplant, they removed most of the recipient’s natural liver to confirm its regenerative abilities. Most recipients of livers stored in cold storage or in the perfusion system with RBCs did not survive, while those transplanted with livers cultured in perfusion system with RBCs showed 100% survival rates for an additional seven days. Normal metabolic functions, such as albumin synthesis and glucose metabolism, were also maintained in the livers cultured in their system with RBCs.
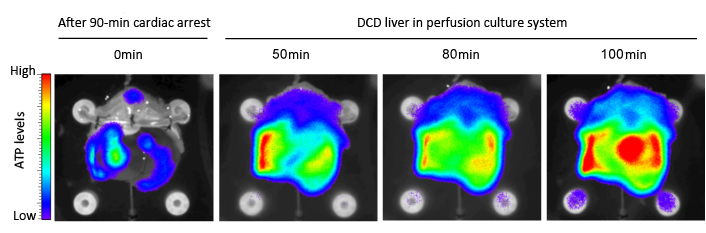
ATP levels in liver drop after cardiac arrest, but recover when placed in perfusion culture system.
Ishikawa et al. also tested whether their perfusion system could be used to resuscitate livers obtained from donors after cardiac arrest. Organs from individuals who have died from cardiac arrest are often not used for organ transplantation as oxygen and energy (ATP) needed for physiological functions are rapidly depleted due to lack of blood circulation to organs (ischemia), leading to tissue damage. They isolated the liver from a rat that had been in cardiac arrest for 90 minutes and placed it in their perfusion culture system with RBCs for 100 minutes. They saw a dramatic drop in ATP levels in the liver after cardiac arrest as expected, but after it was placed in the perfusion culture system, the ATP levels showed a marked increase. Survival rates of recipients of the perfusion culture-treated livers was 100% after 14 days, and even showed regeneration of tissue mass after partial removal of the recipient’s natural liver. Thus, their findings indicate livers extracted from cardiac arrest donors can be resuscitated by the addition of red blood cells to their perfusion culture system maintained at 22°C.
“This study demonstrates that longer organ preservation periods and resuscitation of ischemia-damaged organs is possible using our perfusion culture system,” says Tsuji. “Our next step is to modify the system for pig models, which are genetically closer to humans, with the final goal of making this available for human clinical applications.”
| Link to article |
Hypothermic temperature effects on organ survival and restoration |
|---|